- Research
- Open access
- Published:
Investigation of non-communicable diseases prevalence, patterns, and patient outcomes in hospitalized populations: a prospective observational study in three tertiary hospitals
Journal of Health, Population and Nutrition volume 43, Article number: 128 (2024)
Abstract
Background
Non-communicable diseases (NCDs) pose a significant global health challenge, constituting over 80% of mortality and morbidity. This burden is particularly pronounced in low- and middle-income countries (LMICs), including Ethiopia. Despite this, there’s limited research on this issue in Africa. This study aims to investigate the prevalence, patterns, and outcomes of NCDs in hospitalized populations across three tertiary hospitals in Ethiopia.
Methods
A hospital-based cohort study (August 2022 - January 2023) included patients aged 14 and older diagnosed with cardiovascular diseases (CVDs), diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), asthma, or cancer at three Ethiopian hospitals. Data on demographics, socio-economic factors, clinical characteristics, and outcomes were collected through medical records and interviews. Logistic regression identified factors independently associated with in-hospital mortality, with p ≤ 0.05 considered statistically significant.
Results
In the study across three tertiary hospitals involving 2,237 patients, we uncovered the impact of NCDs. About 23.4% of patients struggled with NCDs, with cardiovascular diseases (53.3%), cancer (29.6%), diabetes (6.1%), and respiratory diseases (6.5%) being the most prevalent. Notably, among those affected, women comprised a slight majority (55.1%), with the average patient age being 47.2 years. Unfortunately, 15.3% of patients with NCDs faced in-hospital mortality. Our analysis revealed predictors of mortality, including cancer diagnosis (adjusted odds ratio [AOR]:1.6, 95% CI: 1.2–1.8, p = 0.01), medication adherence ( AOR: 0.36, 95% CI: 0.21–0.64, p < 0.001), concurrent infections (AOR: 0.36, 95% CI: 0.16–0.86, p < 0.001), chronic kidney diseases (CKD) (AOR: 0.35, 95% CI: 0.14–0.85, p = 0.02), and complications during hospitalization (AOR: 6.36, 95% CI: 3.45–11.71, p < 0.001).
Conclusion
Our study reveals a substantial prevalence of NCDs among hospitalized patients, affecting approximately one in four individuals, primarily with CVDs and cancer. Alarmingly, a significant proportion of these patients did not survive their hospitalization, emphasizing the urgent need for targeted interventions to enhance outcomes in this population.
Background
Non-communicable diseases (NCDs) have emerged as a pressing global health challenge, imposing a significant burden of morbidity and mortality [1]. NCDs are the leading cause of death globally, claiming 41 million lives annually, which accounts for 71% of all global fatalities. Four major culprits contribute to over 80% of premature NCD-related deaths: cardiovascular diseases (CVDs), causing 17.9 million deaths annually, cancer (9.0 million), respiratory diseases (3.9 million), and diabetes (1.6 million) [2, 3]. They disproportionately affect low- and middle-income countries (LMICs), particularly in Sub-Saharan Africa [4]. Over the past two decades, NCDs, driven by cardiovascular risk factors like unhealthy diets, inactivity, hypertension, obesity, diabetes, high cholesterol, and air pollution, have surged in this region [5, 6]. Projections suggest that NCDs are on a trajectory to surpass the combined impact of communicable, maternal, neonatal, and nutritional (CMNN) diseases, becoming the leading cause of mortality in Sub-Saharan Africa by 2030 [7, 8].
The surge in NCDs within LMICs is propelled by population ageing, rapid urbanization, and lifestyle changes [9]. Additionally, many LMICs, including Ethiopia, face a high incidence of communicable diseases and an overburdened healthcare system, intensifying the impact of NCDs, such as premature mortality [10]. Approximately 48% of NCDs in LMICs occur in individuals below the age of 70, compared to 28% in high-income countries (HICs) [11]. Ethiopia, in East Africa, is experiencing significant demographic and epidemiological transformations [12]. Rapid urbanization, globalization, and climate change are shaping the country’s evolving landscape [13, 14].Despite government initiatives like the 2003 health extension program improving life expectancy and reducing infectious, maternal, and child deaths, Ethiopia faces challenges from a shifting population pyramid [12]. Socio-economic shifts, lifestyle changes, and globalization have initiated a nutrition transition from traditional, healthful diets to processed and fast foods [15,16,17]. Consequently, Ethiopia is undergoing an epidemiological shift from communicable diseases to chronic conditions [12].
Hospitalized populations, dealing with complex health conditions, require intensive medical attention, and the burden of NCDs significantly strains healthcare systems, particularly during hospitalizations. Previous studies using Health Information Management System (HMIS) data have shown rising trends in NCDs among inpatients in developed eastern coastal China [18], Nepal [19], Nigeria [20] and Myanmar [21].
While considerable research has been conducted on NCDs in Ethiopia [9, 22, 23], there is a gap in understanding the prevalence, patterns, and outcomes associated with these diseases specifically within hospitalized populations. This research aims to address this gap by investigating the prevalence, evolving patterns, and outcomes of NCDs during hospitalization. Identifying such nuanced information is vital for informing targeted interventions, optimizing healthcare resource allocation, and improving the overall quality of care for individuals affected by NCDs in hospital settings.
Methods and materials
Study area
The study was conducted at three healthcare facilities in Addis Ababa, Ethiopia: Tikur Anbessa Specialized Hospital (TASH), St. Paul Hospital Millennium Medical College (SPHMMC), and Yekatit 12 Hospital (YH). TASH, established in 1972, is the largest referral hospital in Ethiopia. It serves a diverse population with varying socio-economic and demographic backgrounds and offers a wide range of specialized clinical services. SPHMMC, founded in 1968, operates as a teaching hospital with a bed capacity of 700 and initiated Ethiopia’s first integrated modular and hybrid problem-based curriculum for undergraduate medical education in 2007. YH, established in 1923, is also a tertiary-level referral and teaching hospital that provides comprehensive inpatient and outpatient care, serving a large population from both the city and different parts of the nation, including cancer patients.
Study design and period
This was a prospective observational follow-up focusing on patients admitted to the internal medicine, gynaecology and obstetrics and oncology wards during the follow up period from August 2022 to January 2023. We followed-patients until death or discharged to different area (intensive care unit, home, other institution, and wards).
Study population
The study included all eligible patients admitted to the internal medicine, gynaecology, obstetrics, and oncology wards at TASH, SPHMMC, and YH, covering various NCDs such as heart failure, coronary heart disease, cerebrovascular disease, atrial fibrillation, peripheral arterial disease, rheumatic heart disease, hypertension, deep vein thrombosis, pulmonary embolism, cancer (both solid and liquid tumours), and chronic respiratory diseases (asthma and COPD).
Inclusion criteria and exclusions in patient selection
We included patients aged 14 years and older with confirmed NCDs diagnoses in our study. In our facility, adolescent patients in this age group are admitted to adult wards as there is no separate ward for them, and they receive treatment in a manner similar to adults. We chose to incorporate them into our research due to their willingness to cooperate and respond to interview questionnaires. Patients aged less than 14 years as well as those who declined to participate or had incomplete medical records were excluded from the study.
Study variables
Dependent variables: Proportion of NCDs among hospitalized population during study period = (number of admitted patients with NCDs / total number of admissions) x 100. Other dependent variables included were mortality, length of hospital stay, readmission rate within 30-day of discharge, and complications and prescription patterns of key drugs at discharge. Complication was defined as any conditions the patients developed during hospital stay such as hospital acquired infection, bleeding, adverse reaction to medications, organ failure (e.g. acute renal injury, respiratory failure, delirium, etc…). Independent variables: Age, gender, socio-economic factors (monthly income, education and employment), lifestyle factors (physical activity), behavioural factors (drinking and smoking habits), marital status, residency (urban/rural), family history of NCDs, self-reported adherence to medications and concomitantly occurring conditions.
Data collection tool
The data collection process was carried out using a comprehensive tool specifically designed in accordance with the study objectives and tailored to the local context. This tool was designed to gather detailed demographic information, medical history, lifestyle factors, and clinical outcomes of patients admitted with non-communicable diseases. The instrument was based on established clinical assessment protocols, validated questionnaires (such as the World Health Organization (WHO) STEPS questionnaire for risk factors assessment), and electronic health record data extraction templates. Three trained nurses and 3 pharmacists collected data using standardized procedures, ensuring consistency and reliability. Patients admitted with NCDs, including CVDs, DM, chronic respiratory diseases, and cancers, were included in the data collection process. The quality of the data collection tool was assessed through pilot testing, inter-rarer reliability checks, and on-going monitoring to ensure accuracy and completeness of data. Additionally, regular training sessions and supervision were provided to maintain data collection standards and address any challenges encountered during the study period.
Data analysis
Continuous variables (age, monthly income, length of hospital stay) were presented as mean (SD) or median with interquartile range (IQR), while categorical variables (gender, occupation, marital status, place of residence, family history, current smoking status, alcohol drinking status, physical activity, medication adherence, concomitant infection during admission, CKD, epilepsy, readmission within 30 days of discharge, complication during hospital stay, mortality) were expressed as percentages and frequency. The chi-squared test assessed associations between mortality and different NCDs. Binary and multivariate logistic regression analyses, including variables with p-values < 0.2 in univariate analysis, identified predictors of mortality. Significance was set at p ≤ 0.05, and results were reported with 95% confidence intervals. SPSS version 25 facilitated data analysis.
Ethical clearance
Ethical approval was obtained from the School of Pharmacy, College of Health Sciences at Addis Ababa University Ethical Review Committee. Permissions were also sought from each department involved. Informed consent was obtained from all study participants, who were fully informed about the study objectives and given the option to decline or participate. Patient identification numbers were used instead of names to ensure confidentiality.
Results
Baseline characteristics of the included patients
Our study covered a total of 2,237 inpatient visits across three distinct medical institutions in Ethiopia: Tikur Anbessa Specialized Hospital (TASH, n = 1,111), Yekatit 12 Hospital (YH, n = 671), and St. Paul’s Hospital Millennium Medical College (SPHMMC, n = 455). These data were collected over the period from October 2022 to January 2023. Within this patient cohort, 523 admissions were attributed to a range of NCDs, including (CVDs, n = 279, 53.3%), cancer (n = 155, 29.6%), (DM, n = 32, 6.1%), respiratory diseases (n = 34, 6.5%), and a combination of CVDs and DM (n = 23, 4.4%). Consequently, the proportion of patients with NCD among hospitalized patients within our sample was calculated as 23.4% (523 out of 2,237).
Table 1 presents characteristics of patients hospitalized with NCDs. Admissions were distributed across TASH (49%), SPHMMC (27.5%), and YH (23.5%). Gender leaned slightly female (55.1%), with middle-aged adults (51.1%) being the most common age group. The mean average age of the patients was 47.2 ± 18.1. Most patients were urban (76.9%) and married (66.2%). Education varied, with many completing primary school (33.5%) or college/university (26%). Notably, 36.3% reported monthly incomes exceeding $100, while smaller percentages reported ‘no income’ (1.3%), ‘refused to tell’ (11.3%), or ‘I do not know’ (6.5%), indicating income uncertainty among some respondents. The median range of monthly income of the participants was $88.4 (IQR = $33-$154). Additionally, about 31.5% of patients had a family history of at least one NCD. Few engage in regular physical activity (6.5%). The majority of patients exhibit an extensive disease history, accounting for 97.9% (512 individuals). The median duration since diagnosis stands at 12 months, with an IQR spanning from 2 months to 48 months. In terms of concurrent health conditions accompanying NCDs, it was observed that 28.5% of patients presented with additional medical issues during their hospitalization. Among these co-existing conditions, infections of various types were the most prevalent (27.5%), followed by CKD (24.8%) and tuberculosis (12.6%).
Patterns of NCDs among inpatient by demographic and socio-economic characteristics
Among male participants, the most prevalent NCD among hospitalized patients was CVDs at 52.3%, followed by cancer (31.5%). Similarly, female participants exhibited CVDs as the predominant NCD at 54.5%, followed by cancer (27.8%) (Fig. 1).
Patterns of NCD in hospitalized patients by demographic and socioeconomic characteristics. NCD: Non-Communicable Disease, CVD: Cardiovascular Disease, DM: Diabetes Mellitus, RD: Respiratory Disease. *Included patients with no reported income [7], those who were uncertain (59), and those who refused to disclose their income [34]
A higher percentage of hospitalized seniors were having CVDs (67.2%), with middle-aged adults also showing a substantial proportion (50.2%), whereas a relatively lower percentage of adolescent and young adults were having CVD (48.6%). Conversely, with cancer a larger percentage comprises adolescent and young adults (42.1%), followed by middle-aged adults (30.3%), with a significantly lower representation among senior adults (12.1%) (Fig. 2). Overall, CVDs and cancer comprised 82.9% of NCDs among admitted patients.
Regardless of education, CVDs were the most common conditions, ranging from 51.3 to 55.7% in different education groups, followed by cancer. Retired individuals had the highest rate CVDs at 68.0%, while employed and unemployed patients showed similar NCD admission proportions, with more cancer cases among the unemployed. Overall, CVDs affected the majority (53.5%).
In our study, heart failure emerged as the predominant CVD in hospitalized patients, representing 35.1% of cases, followed by stroke at 14.3%. Notably, heart failure combined with chronic rheumatic valvular heart disease contributed to 10.1% cases, while venous thromboembolism and hypertension accounted for 9.7% and 3% of cases, respectively. Additionally, coronary heart diseases were responsible for 2.3% of the total cases (Fig. 3). Primary cancer types among the hospitalized patients were predominantly haematological cancers, encompassing approximately 105 cases, which represented 67.7% of all cancer-related admissions. Within this category, acute lymphoblastic leukaemia (ALL) had the highest representation at 27.7%, followed by acute myeloid leukaemia (AML) at 18.7%, and chronic lymphocytic leukaemia (CLL) at 12.9%. In the realm of solid tumours, cervical cancer was the most prevalent at 8.4%, followed by ovarian cancer (8.4%) and breast cancer (3.2%) (Fig. 4). Among respiratory disorders, asthma prevailed, affecting 70.6% of respiratory cases, while chronic obstructive lung diseases were present in 29.4% of hospitalized patient population. Furthermore, our analysis revealed the most common combination of CVDs and DM resulting was heart failure with DM, representing 52.2% of cases. Hypertension with DM and coronary heart diseases with DM followed closely at 17.4% each, while peripheral artery disease contributed to 8.7% of the cases. The combination of dyslipidaemia and DM was the least common, accounting for 4.4% of cases.
Frequency of CVDs among hospitalized patients. *Heart failure + atrial fibrillation [5], Heart failure + coronary heart diseases [6], Atrial fibrillation [2], Atrial fibrillation + rheumatic heart disease [6], Hypertension + stroke [9], Rheumatic heart disease [7], Heart failure + venous thromboembolism [6], Heart failure + asthma [1], Coronary heart diseases + peripheral artery disease [2], Heart failure + atrial fibrillation + rheumatic heart disease [3], Heart failure + hypertension [8], Peripheral artery disease [1], Dyslipidemia [1]
Prescription pattern of discharge medications
In our CVD patient group, diuretics were the most common discharge medications (37.9%, n = 198), followed by anticoagulants (36.5%, n = 191), and statins (24.1%, n = 126). Notably, 9.2% (n = 48) required insulin for DM management. Among patients with respiratory conditions, the primary choice was short-acting beta-agonists (6.1%, n = 32), followed by inhalation corticosteroids (4.8%, n = 25). Oral corticosteroids were less common, with only 2.7% (n = 14) of prescriptions (Fig. 5).
Outcomes of patients admitted due to NCDs
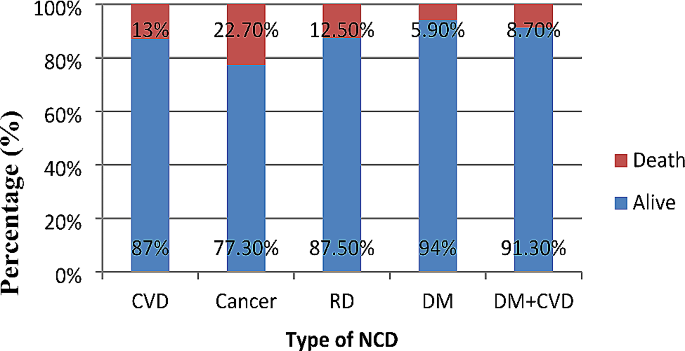
Eighty individuals (n = 80, 15.3%) did not survive the hospitalization. For those patients who survived (n = 443, 84.7%), a significant portion, approximately 405 individuals (77.4%), were discharged and able to return to their homes. A smaller subgroup, comprising around 10 patients (1.9%), necessitated admission to the intensive care unit (ICU) during their hospitalization. Additionally, roughly 16 patients (3.1%) were transferred to other wards within the hospital, while approximately 12 patients (2.3%) were referred to external healthcare institutions for further medical attention. Within the study period, 7.5% of the admitted patients experienced readmission, and 38.8% developed complications during their hospital stay (Fig. 6). Furthermore, the analysis revealed that the median duration of hospitalization for all patients in the study was 9 days, with a notable interquartile range of 6–15 days.
Relationship between NCD and mortality in hospitalized patients
Figure 7 illustrates various patterns of in hospital-mortality among hospitalized patients with NCDs. Among these patterns, cancer exhibited the highest mortality rate at 22.7%, followed by CVDs at 13%, DM at 12.5%, and respiratory disorders with the lowest mortality rate of 5.9%. Statistical analysis indicates a significant association between NCDs related hospital admission and patient mortality (χ2 = 10.8, p = 0.02).
Predictors of mortality in patients with NCDs
Patients with cancer had 50% more mortality compared to patients with CVDs (AOR: 0.5, 95%CI: 0.2–0.8, p = 0.01]. Patients who adhered to their outpatient prescribed medications were 64% less likely to die compared to non-adherent patients (AOR: 0.36, 95% CI: 0.21–0.64, p < 0.001). Patients without infection had a 64% lower risk of mortality compared to those with infection (AOR: 0.36, 95% CI: 0.16–0.86, p < 0.001). Patients without CKD had a 65% lower risk of mortality compared to patients with CKD (AOR: 0.35, 95% CI: 0.14–0.85, p = 0.02). Furthermore, patients with complications during their hospital stay were about 6.4 times more likely to die compared to patients without complications (AOR: 6.36, 95% CI: 3.45–11.71, p < 0.001) (Table 2).
Discussion
In settings where community-based studies and comprehensive data on NCDs are lacking, hospital-based studies serve as vital tools for evaluating the health status of the community served by the hospital. Our study on the patterns of NCDs among hospitalized patients provides valuable insights into the complex interplay of various factors influencing disease prevalence and outcomes.
Our findings highlight that CVDs and cancer collectively constitute a substantial 82.3% of NCD cases among hospitalized patients. This observation is consistent with similar studies conducted in Ethiopia and other African countries [22, 24,25,26]. However, contrasting findings from a study in Nigeria show that CVDs, endocrine, and renal conditions collectively comprise the majority (78%) of NCD cases [27].The variance in findings underscores the influence of regional and contextual factors on disease prevalence. It is noteworthy that our study encompassed a broader spectrum of specialities, including gynaecology, obstetrics, oncology, and medical wards, which may account for differences in disease rankings compared to studies focused solely on medical wards in Nigeria. This broader scope is particularly significant in countries like Ethiopia, which face dual health challenges of communicable diseases such as HIV, tuberculosis (TB), and malaria alongside a rising burden of NCDs [28].
The age-specific analysis from our study reveals a higher prevalence of hospital admissions for NCDs among younger cohorts (under 64 years) compared to seniors (aged 65 years and older). This finding aligns with international research trends, such as studies conducted in Sweden, indicating a global pattern where younger adults are more frequently hospitalized for NCDs compared to older adults [29]. The implications underscore the importance of age-specific healthcare strategies for effective NCD management and prevention.
Regarding specific disease entities, our study found that seniors and middle-aged adults exhibit higher hospitalization rates for CVDs, whereas young adults show a higher prevalence of cancer among admitted patients. This observation reflects the cumulative nature of CVD development with age, influenced by factors such as blood pressure, cholesterol levels, and atherosclerosis, whereas cancers prevalent in younger adults, such as leukaemia and lymphoma, exhibit distinct risk profiles [30, 31].
Within the arena of CVDs, heart failure emerges as the predominant condition among hospitalized patients, consistent with findings from studies across diverse geographical regions [32, 33]. Stroke also stands out as a significant contributor to cardiovascular-related admissions, underscoring its impact as a leading cause of hospitalization in neurology departments [34]. Additionally, another study highlights stroke as a notable cause of admission to a tertiary care centre [35]. These findings emphasize the critical need for interventions addressing heart health, particularly in cases where heart failure coincides with chronic rheumatic valvular heart disease, as noted in prior research [36]. Similarly, our study underscores the importance of early detection and treatment for primary cancer types, such as ALL, AML, CLL, and cervical cancer. These insights are crucial for guiding targeted healthcare interventions aimed at improving cancer outcomes among hospitalized patients.
Our study also reports an in-hospital mortality rate of 15.3% among patients with NCDs, with cancer exhibiting the highest case fatality rate at 22.7%, followed by CVDs at 13%, and DM at 12.5%. These mortality patterns align with global trends reported by the World Health Organization (WHO), highlighting the substantial burden of NCDs worldwide [37]. Variations between our findings and WHO data may be attributed to the inclusion of younger individuals in our study, potentially underestimating CVD burdens while highlighting haematological tumours. Comparative studies from Sudan and northern Ethiopia reinforce our findings, indicating high case fatality rates associated with malignancy, sepsis, neurological diseases, and CVDs among hospitalized patients [25, 26]. These parallel findings underscore the urgent need for enhanced healthcare strategies to improve patient outcomes and mitigate the impact of NCDs.
These collective results underline the urgency of focusing on NCDs management and prevention strategies to mitigate their impact and improve patient well-being. A distinct set of findings emerged from a retrospective study in Nigeria that involved 2,922 participants. In this study, CVDs were responsible for the highest proportion of NCD-related deaths, constituting 33.5% of the cases [25]. The divergence in results between our study and the Nigerian study could be attributed to several factors. Notably, our study encompassed a wider range of medical wards, including medical, gynaecology, obstetrics, and oncology wards, while the Nigerian study focused solely on medical wards. This broader scope in our study might have contributed to the variations in the reported causes of NCD-related mortality, emphasizing the impact of the diversity of ward inclusions on the outcomes.
In addressing mortality risks, our study underscores the significance of medication adherence, infection control, and co-morbidity management. Elevated mortality risks associated with infections and chronic kidney disease (CKD) highlight the critical need for proactive infection control measures and comprehensive co-morbidity management strategies. Similar findings have been documented in studies focusing on renal diseases and hospital complications [24, 26].
The findings have significant implications.
-
1.
For clinical practice.
-
a.
CVDs and cancer collectively accounted for 82.3% of all NCD cases, underscoring their substantial impact in Africa. Younger adults (under 64) exhibited higher hospitalization rates for NCDs compared to older adults, revealing a global health trend. Heart failure predominated among CVDs, while stroke emerged prominently in neurology departments.
-
b.
Cancer ranked as the second most common NCD among hospitalized patients, highlighting the urgent need for enhanced cancer care. The high case fatality rate of cancer (22.7%) emphasizes the importance of improving treatment outcomes.
-
2.
From a public health perspective.
-
a.
It is essential to prioritize preventive health strategies and enhance healthcare infrastructure to effectively manage prevalent NCDs. Health education initiatives can empower communities with knowledge about disease prevention and early detection, potentially reducing disease burden.
-
b.
Implementing evidence-based policies is crucial for improving clinical care, mitigating the impact of NCDs, and enhancing overall patient outcomes. These efforts aim to foster healthier communities by addressing the root causes and management of NCDs comprehensively.
Strengths and limitations
Despite its strengths, our study has several limitations. Firstly, the study was conducted exclusively in Addis Ababa, Ethiopia, across three healthcare facilities, potentially limiting the generalizability of findings to other regions. Secondly, the inclusion of adolescents in adult wards may influence health profiles and outcomes compared to dedicated paediatric wards. Thirdly, while socio-economic factors like income and education were considered, other factors such as healthcare access and insurance status were not included, which could impact NCD outcomes. Lastly, the exclusion of patients with rare or emerging NCDs or multiple co-morbid conditions may limit the comprehensive understanding of NCD patterns among hospitalized patients. Despite the study limitations, its prospective design, inclusion of diverse wards, and use of established data tools (WHO STEPwise) strengthen its validity and contribute valuable insights into NCD among hospitalized patients and their outcomes in the study area.
Conclusion
In conclusion, our study provides critical insights into predictors of mortality among hospitalized patients with NCDs. By examining a diverse cohort across multiple specialty wards, we have identified significant associations between cancer diagnosis, medication adherence, infections, CKD, and hospital complications with increased mortality risks. These findings underscore the multifaceted nature of NCD management and highlight the importance of targeted interventions to improve patient outcomes in hospital settings. Moving forward, efforts to enhance medication adherence, infection control measures, and co-morbidity management can potentially mitigate mortality rates among individuals with NCDs, thereby advancing healthcare delivery and patient outcomes in hospital settings. Overall, our study contributes to advancing the understanding of NCD epidemiology and clinical management, with implications for improving healthcare practices and policies aimed at combating NCDs globally.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- NCD:
-
Non-communicable disease
- CVD:
-
Cardiovascular disease
- DM:
-
Diabetes mellitus
- COPD:
-
Chronic obstructive pulmonary disease
- CKD:
-
Chronic kidney disease
- CMNN:
-
Communicable, maternal, neonatal, and nutritional
- TASH:
-
Tikur Anbessa specialised hospital
- SPHMMC:
-
St. Paulos hospital Millennium medical college
- YH:
-
Yekatit 12 hospital
- ICU:
-
Intensive care unit
- LMICs:
-
Low- and middle-income countries
- SD:
-
Standard deviation
- IQR:
-
Interquartile range
- WHO:
-
World health organization
- AML:
-
Acute myeloid leukaemia
- CLL:
-
Chronic lymphoblastic leukaemia
- ALL:
-
Acute lymphoblastic leukemia
- HIV:
-
Human immunodeficiency virus
- TB:
-
Tuberculosis
References
Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. The Lancet (2018) 22;(392):1072–88.
Ramesh S, Kosalram K. The burden of non-communicable diseases: a scoping review focus on the context of India. J Educ Health Promot. 2023;12:41. https://doi.org/10.4103/jehp.jehp_1113_22.
Mohammad HF. 2015. Global, regional, and national comparative risk assessment of 79 behaviournvironmental and occupational, and metabolic. risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet (2016);388(10053):1659–724.
Ezzati M, Pearson-Stuttard J, Bennett JE, Mathers CD. Acting on non-communicable diseases in low- and middle-income tropical countries. Nature. 2018;559(7715):507–16.
Idris IO, Oguntade AS, Mensah EA, Kitamura N. Prevalence of non-communicable diseases and its risk factors among Ijegun-Isheri Osun residents in Lagos State, Nigeria: a community based cross-sectional study. BMC Public Health. 2020;20:1258.
Mudie K, Jin MM, Tan null, Kendall L, Addo J, Dos-Santos-Silva I, et al. Non-communicable diseases in sub-saharan Africa: a scoping review of large cohort studies. J Glob Health. 2019;9(2):020409.
Bigna JJ, Noubiap JJ. The rising burden of non-communicable diseases in sub-saharan Africa. Lancet Glob Health. 2019;7(10):e1295–6.
WHO. 2023. Non communicable diseases [Internet]. [cited 2023 Oct 17]. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
Girum T, Mesfin D, Bedewi J, Shewangizaw M. The Burden of Noncommunicable Diseases in Ethiopia, 2000–2016: Analysis of Evidence from Global Burden of Disease Study 2016 and Global Health Estimates 2016. International Journal of Chronic Diseases (2020) 20;2020:e3679528.
Organization WH. Global status report on noncommunicable diseases 2010. 2011 [cited 2023 Nov 16]; https://iris.who.int/handle/10665/44579.
WHO. 2014. Global status report on noncommunicable diseases 2014 [Internet]. [cited 2023 Nov 16]. https://www.who.int/publications-detail-redirect/9789241564854.
Alamnia TT, Sargent GM, Kelly M. Patterns of non-communicable Disease, Multimorbidity, and Population Awareness in Bahir Dar, Northwest Ethiopia: a cross-sectional study. Int J Gen Med. 2023;16:3013–31.
Juma K, Juma PA, Shumba C, Otieno P, Asiki G, Juma K et al. Non-Communicable Diseases and Urbanization in African Cities: A Narrative Review. In: Public Health in Developing Countries - Challenges and Opportunities [Internet]. IntechOpen; 2019 [cited 2023 Nov 16]. https://www.intechopen.com/chapters/69370.
Misganaw N. Walker, Mirkuzie, Giref, Berheto, et.al. Progress in health among regions of Ethiopia, 1990–2019: a subnational country analysis for the global burden of Disease Study 2019. Lancet. 2022;399(10332):1322–35.
Bosu WK. An overview of the nutrition transition in West Africa: implications for non-communicable diseases. Proc Nutr Soc. 2015;74(4):466–77.
Mbogori T, Kimmel K, Zhang M, Kandiah J, Wang Y. Nutrition transition and double burden of malnutrition in Africa: a case study of four selected countries with different social economic development. AIMS Public Health. 2020;7(3):425–39.
Popkin BM. The Nutrition Transition in the developing World. Dev Policy Rev. 2003;21(5–6):581–97.
Yu D, Shi J, Zhang H, Wang Z, Lu Y, Zhang B, et al. Identifying patterns of non-communicable diseases in developed eastern coastal China: a longitudinal study of electronic health records from 12 public hospitals. BMJ Open. 2017;7(10):e016007.
Amundsen MS, Kirkeby TMG, Giri S, Koju R, Krishna SS, Ystgaard B, et al. Non-communicable diseases at a regional hospital in Nepal: findings of a high burden of alcohol-related disease. Alcohol. 2016;57:9–14.
Sani MU, Mohammed AZ, Bapp A, Borodo MM. A three-year review of mortality patterns in the medical wards of Aminu Kano Teaching Hospital, Kano, Nigeria. Niger Postgrad Med J. 2007;14(4):347–51.
Swe EE, Htet KKK, Thekkur P, Aung LL, Aye LL, Myint T. Increasing trends in admissions due to non-communicable diseases over 2012 to 2017: findings from three large cities in Myanmar. Trop Med Health. 2020;48:24.
Odenigbo CU, Oguejiofor OC. Pattern of medical admissions at the Federal Medical Centre, Asaba-a two year review. Niger J Clin Pract. 2009;12(4):395–7.
Memirie ST, Habtemariam MK, Asefa M, Deressa BT, Abayneh G, Tsegaye B, et al. Estimates of Cancer incidence in Ethiopia in 2015 using Population-based Registry Data. J Glob Oncol. 2018;4:1–11.
Hailu A, Gidey K, Ebrahim MM, Berhane Y, Gebrehawaria T, Hailemariam T, et al. Patterns of medical admissions and predictors of mortality in Ayder Comprehensive Specialized Hospital, Northern Ethiopia: a prospective observational study. Int J Gen Med. 2023;16:243–57.
Ogunmola OJ, Olamoyegun MA. Patterns and outcomes of medical admissions in the accident and emergency department of a tertiary health center in a rural community of Ekiti, Nigeria. J Emerg Trauma Shock. 2014;7(4):261–7.
Omar SM, Osman OS, Gasim GI, Adam I. Pattern and Trends in Adult Hospitalization/Admission and mortality among Medical Ward inpatients at Gadarif Hospital in Eastern Sudan: A Four-Year Retrospective Study. Int J Gen Med. 2022;15:5879–89.
Akubudike AC, Eze NC. Non communicable Disease admissions in Developing Country as experienced from the Medical Ward of a Tertiary Centre in Nigeria. Cent Afr J Public Health. 2018;4(2):34.
Bygbjerg IC. Double burden of noncommunicable and infectious diseases in developing countries. Science. 2012;337(6101):1499–501.
Gondek D, Ploubidis GB, Hossin MZ, Gao M, Bann D, Koupil I. Inequality in hospitalization due to non-communicable diseases in Sweden: age-cohort analysis of the Uppsala Birth Cohort Multigenerational Study. SSM - Popul Health. 2021;13:100741.
Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks Associated with gender and aging. J Cardiovasc Dev Dis. 2019;6(2):19.
Zahnreich S, Schmidberger H. Childhood Cancer: Occurrence, Treatment and Risk of Second Primary Malignancies. Cancers (2021);13(11):2607.
Brown JR, Gottlieb SS. Acute decompensated heart failure. Cardiol Clin. 2012;30(4):665–71.
Salah HM, Minhas AMK, Khan MS, Pandey A, Michos ED, Mentz RJ, et al. Causes of hospitalization in the USA between 2005 and 2018. Eur Heart J Open. 2021;1(1):oeab001.
Evelyne AA, Mamadou Z. Current data on the Profile of patients hospitalized for stroke in a Neurology Department in West Africa: Abidjan (Ivory Coast). Am J Psychiatry Neurosci. 2015;3:14.
Kurmi RN, Mandal L, Singh R, Chaudhary PK, Dhungana T, Lamichanne S, et al. Stroke among patients admitted to a Tertiary Care Centre: a descriptive cross-sectional study. JNMA J Nepal Med Assoc. 2023;61(260):305–9.
Limbu YR, Maskey A, MB KC, Malla R, Sharma D, Shrestha NK, A STUDY ON CARDIOVASCULAR DISEASE PATTERN OF ADMITTED CASES IN NEWLY EMERGED NATIONAL HEART CENTRE. J Nepal Med Assoc. 2003;41(141):284–8.
WHO. 2022. World Health Systems Facts. [cited 2023 Oct 17]. https://healthsystemsfacts.org/. https://healthsystemsfacts.org/.
Acknowledgements
Research reported in this publication was supported by the Fogarty International Centre of the National Institutes of Health under Award Number D43 TW011404. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
A.B: Conceived the study, designed the study, collected the data, data analysis, and wrote the initial draft of the manuscript. L.C.K: Conceived the study, designed the study, supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. F.A: data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. H.F: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. S.G: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. M.K: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. S.A.P: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript. M.K.A: supervision, data analysis, wrote the initial draft of the manuscript, revised and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the School of Pharmacy, College of Health Sciences at Addis Ababa University Ethical Review Committee (ERB/SoP/485/14/2022). Permissions were also sought from each department involved. Written informed consent was obtained from all study participants, who were fully informed about the study’s objectives and given the option to decline or participate. Patient identification numbers were used instead of names to ensure confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Belayneh, A., Chelkeba, L., Amare, F. et al. Investigation of non-communicable diseases prevalence, patterns, and patient outcomes in hospitalized populations: a prospective observational study in three tertiary hospitals. J Health Popul Nutr 43, 128 (2024). https://doi.org/10.1186/s41043-024-00599-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41043-024-00599-z